A reader asked “Autoimmune Encephalitis in kids and therapeutic Treatment agents ![]() “. I am aware that the reader deals with a child with autism, so my focus will be in that direction.
“. I am aware that the reader deals with a child with autism, so my focus will be in that direction.
Autoimmune encephalitis is a collection of related conditions in which the body’s immune system attacks the brain, causing inflammation. The immune system produces substances called antibodies that mistakenly attack brain cells.
Brain Institute
Those with CFS/ME knows that ME stands for myalgic encephalomyelitis which leads to the question — what is the difference?
Acute disseminated encephalomyelitis (ADEM) accounts for around 10% of all known cases of encephalitis. ADEM usually affects children and begins after a childhood rash (exanthema), other viral infections or immunizations. There is usually a latent period of days to two to three weeks before symptoms emerge. The illness has been poorly understood and a variety of terminologies used to describe it, these including post-viral, post-infectious or para-infectious.
Acute disseminated encephalomyelitis (ADEM) | The Encephalitis Society
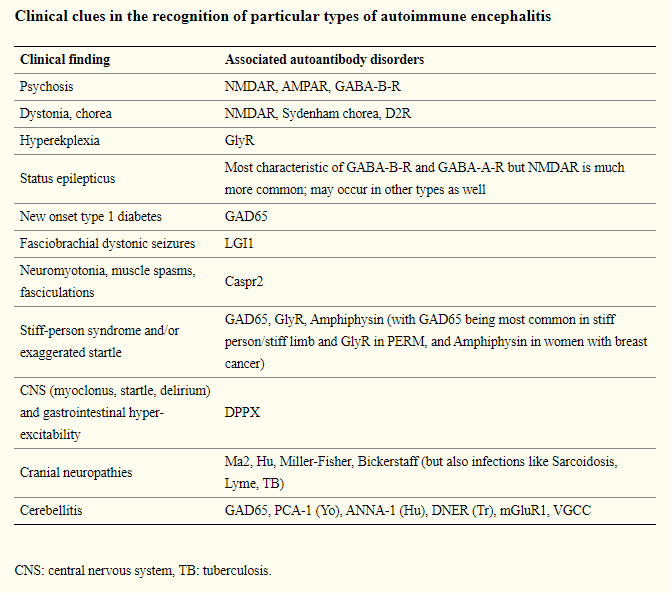
The key words are poorly understood and there is no definitive test to tell them apart. There was a proposal in 2016, A clinical approach to diagnosis of autoimmune encephalitis – autism is not mentioned in this proposal or its appendix. We do see from this article that there are multiple sub-categories.
This article lists the following infection associated: HSV, CMV, VZV, JE, Enterovirus, HHV6, HHV7, Neuroborreliosis (Lyme disease), WNV (West Nile), Syphilis, Cryptococcus, Aspergillus fumigatus, Mucor , Tuberculosis, , Listeria, Streptococcus, Toxoplasmosis. Bold items are items associated to CFS/ME. To these, we need to add COVID.
- Pediatric anti-NMDA receptor encephalitis associated with COVID-19 [2021] Treatment: “pulse steroid treatment was applied”.
- Post-COVID-19 Acute Disseminated Encephalomyelitis in a 17-Month-Old [2021] Treatment: ” high-dose methylprednisolone and intravenous immunoglobulin,”
- COVID-19 and anti-N-methyl-d-aspartate receptor (anti-NMDAR) encephalitis: Are we facing an increase in the prevalence of autoimmune encephalitis? [2021]
- N-Methyl-d-Aspartate Receptor Encephalitis Associated With COVID-19 Infection in a Toddler [2021] Treatment: ” with steroids and intravenous immunoglobulin.”
Autism Specific
“Diagnosing autoimmune encephalitis sooner can increase the effectiveness of curative treatments-such as immune therapy or immune modulatory therapy-that may prevent the long-term consequence of being misdiagnosed with autism spectrum disorder. Glutamate therapy primarily normalizes glutamate neurotransmission and can be a new add-on intervention alongside antipsychotics for treating autoimmune autism.”
Autism Associated With Anti-NMDAR Encephalitis: Glutamate-Related Therapy [2019]
Drilling down in this direction we find:
- Glutamate and functional connectivity – support for the excitatory-inhibitory imbalance hypothesis in autism spectrum disorders – PubMed (nih.gov) [2021] ” excitatory Glx concentrations were related to functional dysconnectivity in ASD.”
- Children with Autism and Their Typically Developing Siblings Differ in Amplicon Sequence Variants and Predicted Functions of Stool-Associated Microbes – PubMed (nih.gov) [2021] Where they use KEGG data
- “Summarizing the expected KEGG orthologs of each predicted genome, the taxonomic biomarkers associated with children with ASD can use amino acids as precursors for butyragenic pathways, potentially altering the availability of neurotransmitters like glutamate and gamma aminobutyric acid (GABA).”
- Cerebral Expression of Metabotropic Glutamate Receptor Subtype 5 in Idiopathic Autism Spectrum Disorder and Fragile X Syndrome: A Pilot Study – PubMed (nih.gov) [2021]
- Developmental changes in fronto-striatal glutamate and their association with functioning during inhibitory control in autism spectrum disorder and obsessive compulsive disorder [2021]
There are a lot more, but the reader’s concern was treatment.
Treatment Options
We have what really amounts to be a symptom ” “, which can be associated with many causes — for example: infections. For those the treatment should be specific for the infection.
For some of the conditions cited above, we have really just one set of suggestions which may be worth considering (after consulting with your medical professional). This is specific for autism, but may be applicable to ME/CFS and Long Haul Covid.
Glutamate supplementation or blockers. See this article Glutamate – The Autism Community in Action (TACA) (tacanow.org). Note that Urine Amino Analysis: (i.e. OATS) and blood tests are deemed unreliable. An old school approach is to insure a stable regular diet and then try supplementation that increases glutamate for 1-2 weeks and then try supplementation that reduces glutamate for 1-2 weeks [see above page]. This will likely provide insight to the nature of the imbalance of glutamate.