Foreword – and Reminder
I am not a licensed medical professional and there are strict laws where I live about “appearing to practice medicine”. I am safe when it is “academic models” and I keep to the language of science, especially statistics. I am not safe when the explanations have possible overtones of advising a patient instead of presenting data to be evaluated by a medical professional before implementing.
I cannot tell people what they should take or not take. I can inform people items that have better odds of improving their microbiome as a results on numeric calculations. I am a trained experienced statistician with appropriate degrees and professional memberships. All suggestions should be reviewed by your medical professional before starting.
Back Story
I enclosed 3 labs: Her last GI MAP, an older OAT, and recent OMBRE.
I have done work since the OAT, obviously.
She was diagnosed with ASD around 20 months old. Since birth severe gastro problems. Re-occurring vomiting and severe GERD. Gastro preformed her first upper scope at age 2.5. He found some food in her stomach. Gave her a gasteopresis diagnosis. At age 5, her second scoop and biopsies and her gasteopresis DX remained. Found nothing on biopsies. Her vomiting stopped once I changed diet by 3 years old. (It was a dairy allergy causing her to vomit once I figured it out, she never vomited again) I don’t believe the GP diagnose fits her and she can’t do the emptying study so he based this dx off food in gut per two scopes.
- PANS/PANDAS dx at age 3.5.
- Has not had a fever since 12 months old.
She is non speaking 6 years old and has cried on and off in pain her whole life. We’ve believed it was her gut from day one . She had a bad smell most of her life coming from her gut.(breathe) I believe this is clostridia as she has tested high with every stool test we’ve ever ran. It got better briefly with a course of abx but came back worse. The smell is the worse when she wakes in the morning. Her stool has always been extremely foul smelling. She has taken some form of probiotics since she was 1 year of age. I have tried to use different strains but my knowledge is limited.
- Severe ear infections since an infant so abx use is very high. 10 times or more.
My next course of action after helping her gut is Lyme and coinfections testing. My research and her latest doctor have lead me there. So if you see anything hinting that way, be very helpful. It’s very expensive testing and I’m just unsure.
Basic Analysis
The usual basics are below:
- Dr. Jason Hawrelak: 95.6%ile on both
- Same sets of bacteria deemed unhealthy, with all of these over 95%ile
- Potential Medical Conditions Detected had some apparent hits:
- ADHD at 96%
- Functional constipation / chronic idiopathic constipation at 95%
- Insomnia and Sleep Apnea likely matches
Clostridia was a specific area of concern, she is at 27.5%ile at the class level. Looking at lower levels we see some if its ‘kids’ are a problem. Three bacteria makes up 60% of the microbiome!
- 4% -> Dorea 97.7%ile
- Dorea longicatena 99.3%ile
- 18.4% -> [Ruminococcus] gnavus 99.7%ile
- 21% -> Blautia 96.1%ile
- 21% -> Ruminococcus bromii 99.9%ile
- 17% -> Acidaminococcus 99%ile
- 26% -> Bifidobacterium 98.4%ile <- Typical with both children, especially with Autism and PANDA
My immediate thought is to look at the suggestions when we hand picked these four. They so dominate the microbiome that trying to adjust the other will likely be shouting in a hurricane (i.e. no one will hear).
Then do a second round including Bifidobacterium
The results we far less than ideal (i.e. very few items over 0.5)
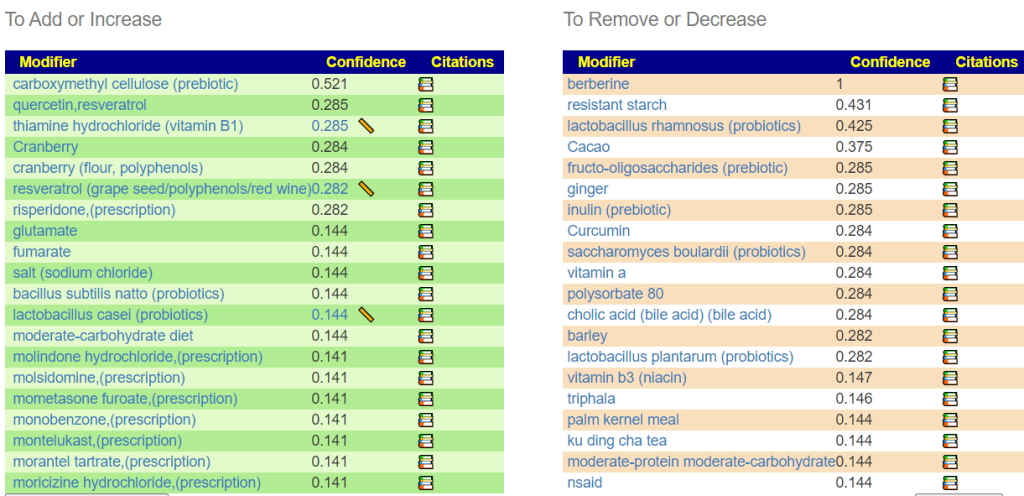
It is interesting that the first prescription items is Risperidone, it is prescribed for irritability caused by autism [more information, including risks]. This hints that there is a match for the bacteria causing irritability in autism. My take away from this list is simple: remove any items on the Avoid list (which includes many vitamins and probiotics “deemed healthy”). bacillus subtilis natto (probiotics) is available is the Japanese desert food Natto (I like it, a bit of an acquire taste) with nattokinase supplement being a potential alternative. The other top items(not prescription) to take are available as supplements etc. I attach the full list.
Adding in Bifidobacterium, we see many items that encourages bifidobacterium on the avoid list.
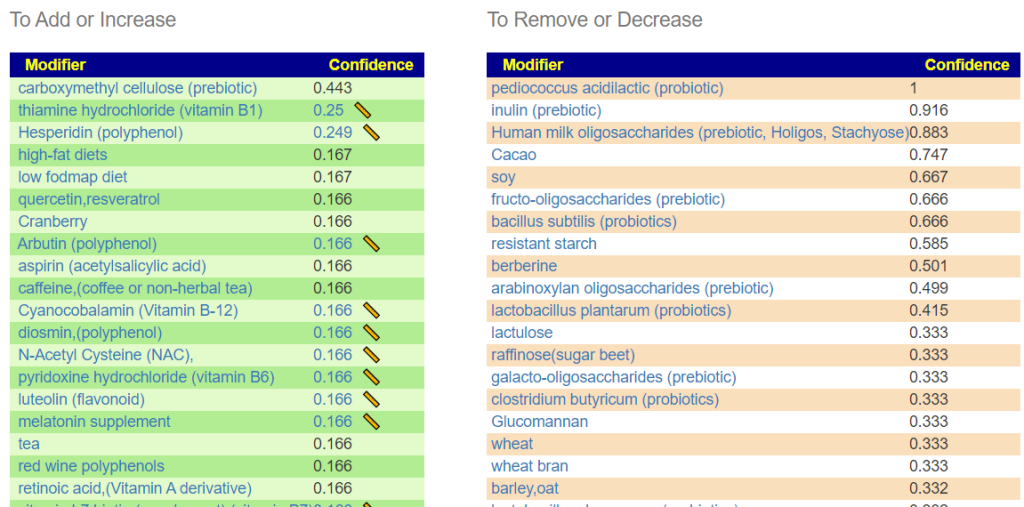
I next did the usual consensus report (which I added to the above sets of suggestions)
- Use JasonH (15 Criteria) – 6 bacteria selected
- Standard Lab Ranges (+/- 2 Std Dev) – 26 bacteria selected
- Box Plot Whisker – 38 bacteria selected
- Kaltoft-Moltrup Normal Ranges – 110 bacteria selected
- Percentile in top or bottom 10% – 136 bacteria selected
The full consensus report is below. Items to TAKE of note:
- melatonin supplement
- blackcurrant — Juice?
- rice
- vegetarians
- thiamine hydrochloride (vitamin B1) and Cyanocobalamin (Vitamin B-12)– seen above
- carboxymethyl cellulose (prebiotic) – this is available pure in bulk,
One item of caution: bacillus subtilis (probiotics) is a strong avoid, one specific species is a moderate take bacillus subtilis natto (probiotics). At the gene levels they are different.
Using KEGG data
Two probiotics showed up at the top that are not available on the shelves of any US Health store: symbiopharm / symbioflor 1 and bioflorin (deu) / bioflorin. In fact, the top items are rich in European probiotics. Symbioflor-1 is available from the German Apotheke and will ship world wide (we use them) as well as bioflorin (which is expensive per capsule, so try symbioflor-1 first for the sake of your wallet!).
In terms of supplements, the following should be reviewed with your MD
- Amylase (Enzyme) – Percentile: 1
- beta-alanine – Percentile: 2.6
- Glycine – Percentile: 2.8
- L-methionine – Percentile: 3.6
- Molybdenum – Percentile: 0.5
- NADH – Percentile: 3.4
Remember that the basis of the KEGG data is identifying compounds that a person is low in. This is based on the hypothesis that part of the microbiome disruption is caused by rationing and impeding the operation of various bacteria. Our data is incomplete — so it is a best estimate.
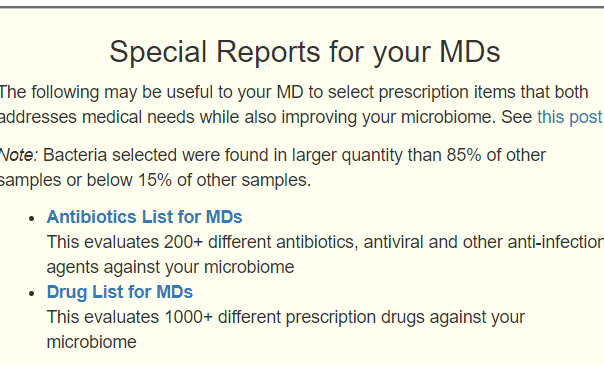
Dive into Antibiotics Taken
I started the easy way — just looking at the Special Reports for your MDs. Everyone given encouraged this child’s dysbiosis.
- Azithromycin for about two months straight at onset of PANS. ( – 0.555 )
- Augmentin (amoxicillin) several times for ear infections and later in life with a functional medicine doctor to address her GI MAP. ( – 0.487 )
- Sulfamethoxazole, ( – 0.642 )
- Vancomycin – increases Acidaminococcus parent
- Cefdinir ( – 0.586 )
There are a small number of antibiotics that may help the microbiome — if antibiotics are required in the future. Discuss if any of these may be acceptable to the MD (i.e. negotiate!) for addressing his rational. Note that the general class macrolide contains both good and bad choices: bad choices (azithromycin), good choices (erythromycin).
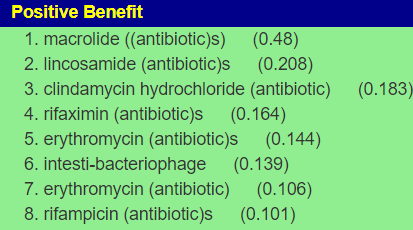
Checking the Positive Benefit for Prescription items, it was very very short. the first suggestion was epinephrine (Adrenaline). This surprised me. A common pattern is too much epinephrine with autism. We need to tread carefully here because levels can be high or low in different parts of the body.
In a group of 22 autistic children aged 5 to 16 years and a group of normal controls matched for age and sex, catecholamines metabolism was investigated in plasma, platelets, and urine. This investigation was part of a research project in which several biological parameters (including serotonin) were explored simultaneously in the same children. In the autistic group, epinephrine and norepinephrine were significantly elevated in plasma, while epinephrine, norepinephrine, and dopamine were significantly lower in isolated platelets. No significant difference was found between the two groups for the urinary excretion of epinephrine, norepinephrine, dopamine, DOPAC, and MHPG. Other differences between the two groups in the statistical correlations of several biochemical parameters also suggest abnormalities of bioamine metabolism in the platelets of autistic children.
Catecholamines metabolism in infantile autism: A controlled study of 22 autistic children
Dive into the key bacteria
Above we have identified the bacteria that has taken over the gut
- [Ruminococcus] gnavus (literature)
- “R. gnavus has been associated with numerous diseases, most prominently inflammatory bowel disease (IBD) ” [src]
- Ruminococcus bromii (literature)
- It feeds especially on resistant starches [src] There are many lists on the web on what these foods are.
- Acidaminococcus (literature)
Questions and Answers
Q: How long do you recommend a follow up stool test after implementing some things?
A: For most things I recommend rotation of suggestions. The purpose is to destabilize the stable dysfunctional microbiome. A typical rotation is 2 weeks. The soonest would be after 4 rotations (2 months), if things are improving then just keep going until things appear to stabilize — then do a new sample to get the next course correction.
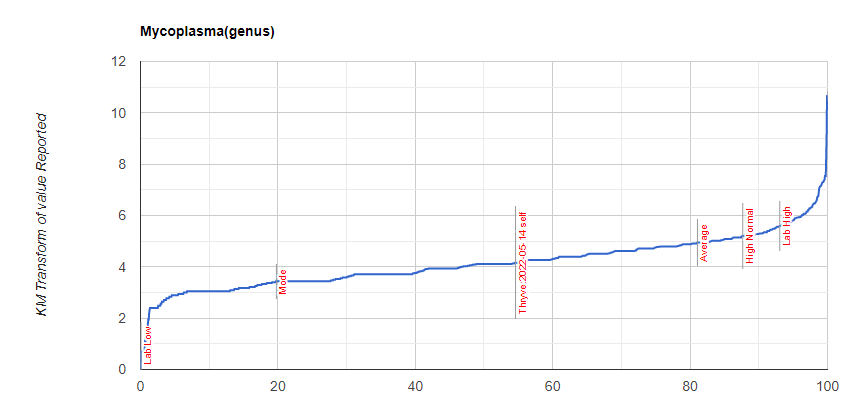
Q: I saw high mycoplasma on the lab’s page – is that a concern? This could explain so much as it is a main trigger for many PANS kids. Did I see that correctly?
A-1: The literature: “Anti-Mycoplasma pneumoniae antibodies and anti-Epstein-Barr virus Nuclear Antigen antibodies were found positive in 11 (42.3%) and 5 (19.2%) patients with PANS,” [2019] This can be tested for directly and that would be the best way to answer.
A-2: Labs (and Microbiome Prescription use different criteria to determine “high”. Your child reading for Mycoplasma was 192 / 1,000,000 bacteria or 57.2%ile. Ombre reports 70% of all samples have some mycoplasma. The level is not abnormal. The chart of values, showing your sample is below
Q: Any evidence of Lyme Disease
A: Lyme is caused by Borrelia. It is reported on Ombre/Thryve tests 0.2% of the time. None was reported in report. Conclusion, unlikely. Given the degree of dysbiosis and the known high rate of false positive with many Lyme tests when there is dysbiosis (typically caused by EBV not being fully controlled due to the dysbiosis), I would say that without a red bull-eye rash on the child — do not bother testing. The antibiotics likely to be prescribe will make your child worst.
